Pertussis
About the pertussis vaccine
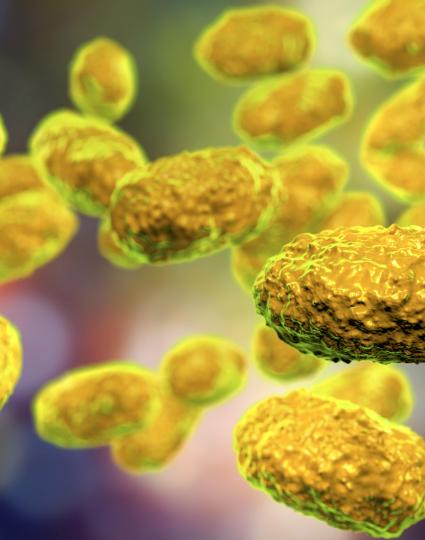
- The pertussis vaccine protects against pertussis, a serious infection of the respiratory system caused by the pertussis bacteria.
- The pertussis vaccine is combined with several other vaccines such as, the Tetanus-Diphtheria-acellular Pertussis (Tdap) vaccine
- It’s included as part of the routine infant and children’s immunization schedule, usually as a 3 dose series.
- Alike other vaccines, pertussis vaccines require a booster to remind your immune system how to fight against pertussis.